Non-Sinus
P wave morphology is not consistent with sinus (including inverted P in lead I)
|
Normal Rate:
|
Fast Rate:
|
Ectopic Atrial Rhythm
- P waves are abnormal in both limb leads and chest leads
CLINICAL SIGNIFICANCE
- Not much
- No treatment is necessary
- Rarely associated with atrial tachycardia
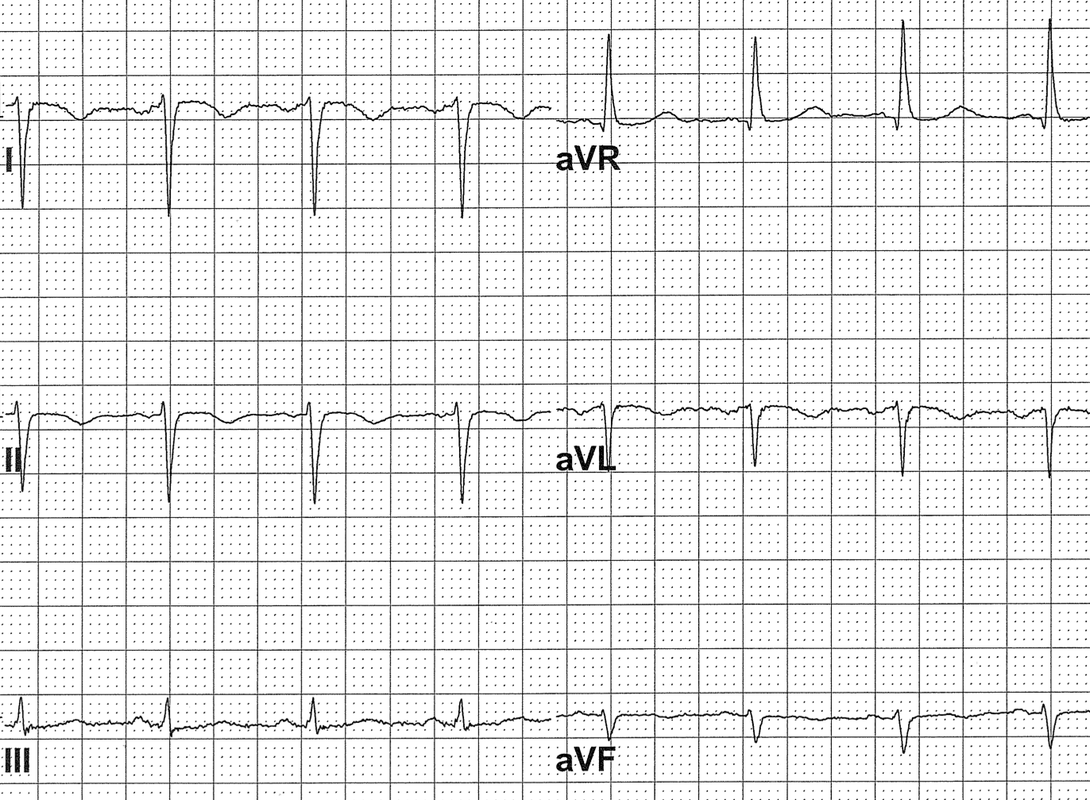
DEXTROCARDIA
- Both P and QRS are inverted in lead I
- QRS progression is reversed in chest leads
CLINICAL SIGNIFICANCE
- ECG is not interpretable and may mimic MIs, fascicular blocks, ischemia
- Repeat ECG with everything reversed
LIMB LEAD REVERSAL
- P waves are normal in the chest leads
- QRS may be inverted in lead I
- Lead II may look like a flat line
CLINICAL SIGNIFICANCE
- Must repeat the ECG!
- Limb leads are bipolar leads
- Limb lead reversal may mimic and mask MIs, fascicular blocks, low voltage, hypertrophy, ischemia
- Lead reversals are very common
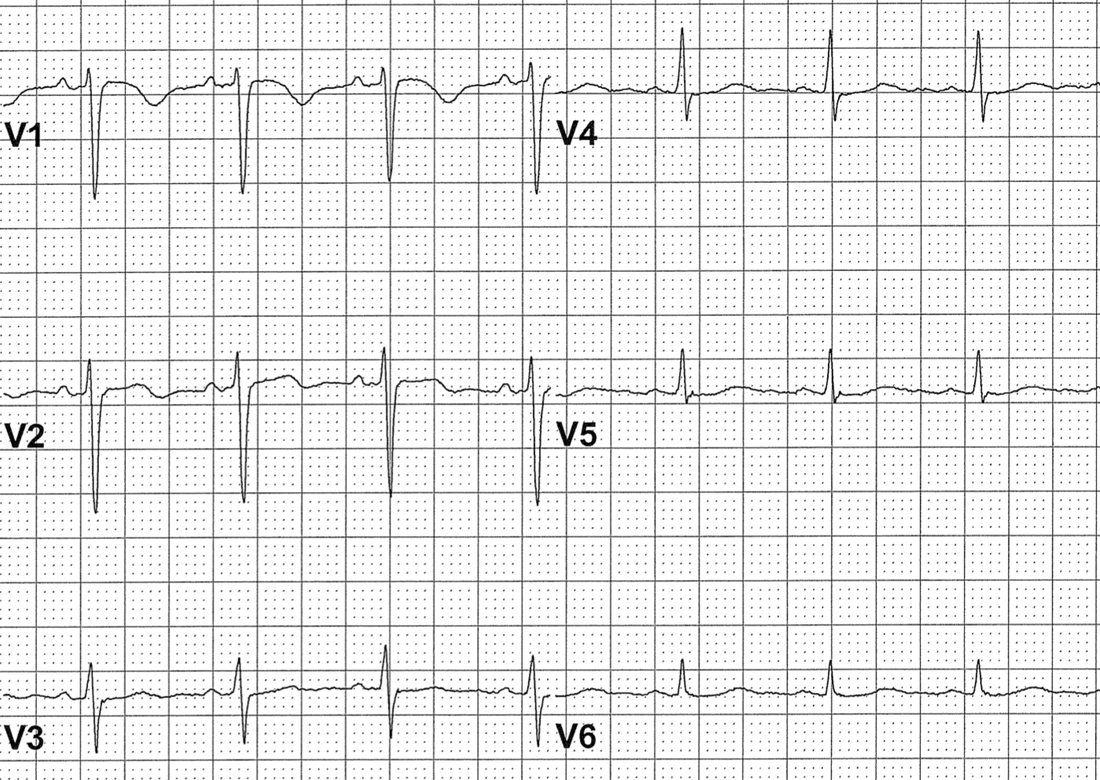
Retrograde P waves
- P waves follow the QRS complexes
- P waves have “retrograde morphology”
- negative in II, III, aVF
- usually upright in V1
- Following junctional QRS complexes
- junctional rhythm or junctional tachycardia
- Following ventricular QRS complexes
- idioventricular rhythm or VT
- Following ventricular paced complexes
CLINICAL SIGNIFICANCE
- When you see an obvious narrow-QRS tachycardia but the computer “thinks” it is a wide-complex tachycardia:
- It is almost always reentrant PSVT where the retrograde P waves are measured as if they were part of the QRS complexes
- Pacemaker Syndrome
- Chest discomfort, shortness of breath related to abnormal pacemaker syndrome
- Most common in ventricular pacing with 1:1 retrograde conduction
- Neck veins: “cannon JVPs”
- Left atrium: “cannon PVPs” (cannot see)
- Either due to ventricular pacer or A-V pacemaker with atrial lead malfunction
- Treatment: upgrade the pacemaker
- Chest discomfort, shortness of breath related to abnormal pacemaker syndrome
Artifact
- Parkinsonian tremor
- High frequency oscillatory ventilation
- Both are typically 5 Hz artifacts
- 5 Hz = 300/min which is the usual atrial rate in atrial flutter
- Clues for distinguishing artifact from flutter:
- Flutter waves are typically sharp
- Flutter waves are typically negative in II, III, aVF
- Sinus P waves are present
CLINICAL SIGNIFICANCE
- Parkinsonian tremor and HFOV are frequently mistaken for Atrial Flutter
- Inappropriate treatments including electric cardioversion have been described
Ectopic Atrial Tachycardia
- Atrial rate 110-220
- P wave morphology is abnormal in the limb leads and the chest leads
CLINICAL SIGNIFICANCE
- Usually a marker of “sickness”
- Usually does not require treatment
- difficult to suppress
- ventricular rate equals atrial rate
- Anticoagulation is usually not indicated
Atrial Flutter
- Atrial rate 230-380
- Extremely common arrhythmia in sick hospitalized patients
- Flutter waves are typically sharp and negative in leads II, III and aVF
- Flutter waves are typically upright in V1
- Atrial Flutter with 2:1 conduction is the most common regular SVT outside of sinus tachycardia in hospitalized patients
Multiple P Wave MOrphologies with Variable PR Intervals
- Rate <100: wandering atrial pacemaker
- Rate >100: multifocal atrial tachycardia
- Frequently read as atrial fibrillation
- Frequently associated with decompensated lung disease, critical illness, postoperative state
- No anticoagulation, no digoxin, no cardioversion
- May treat with diltiazem or beta blocker if symptomatic