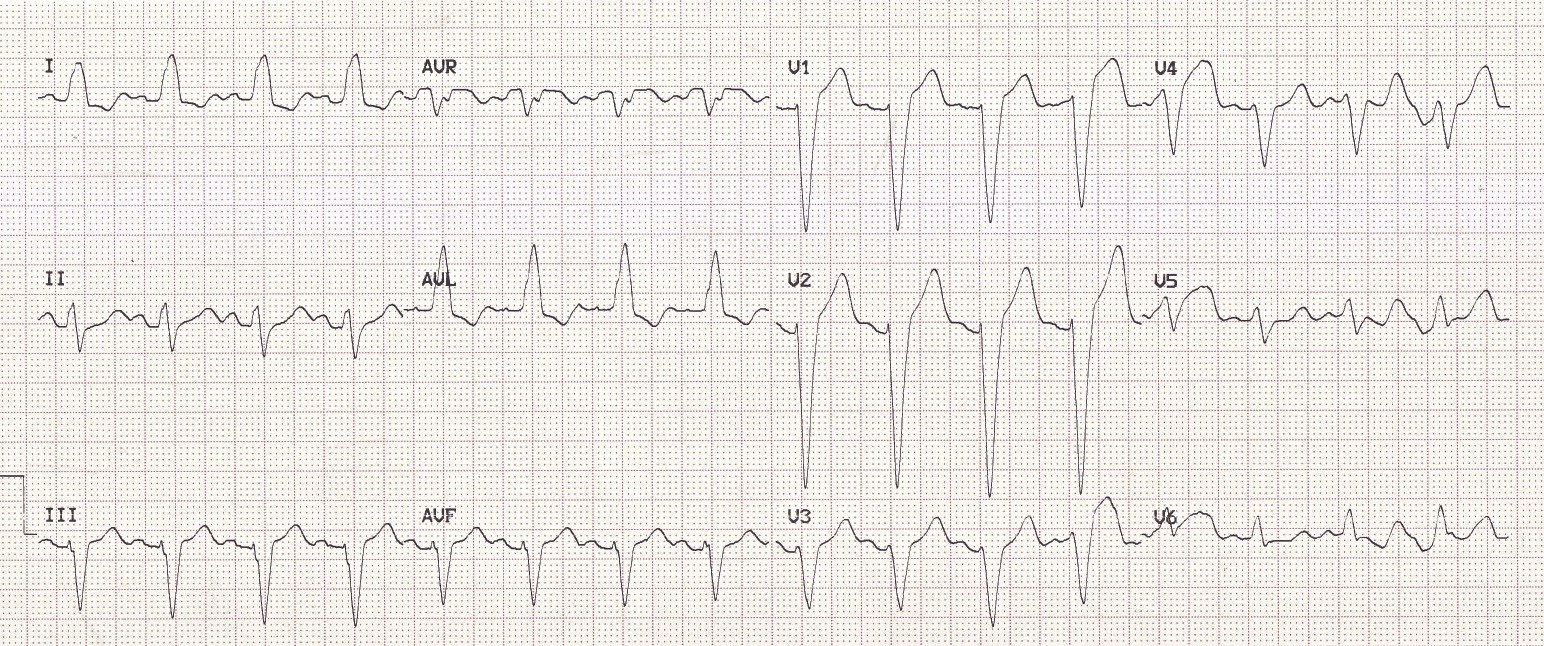
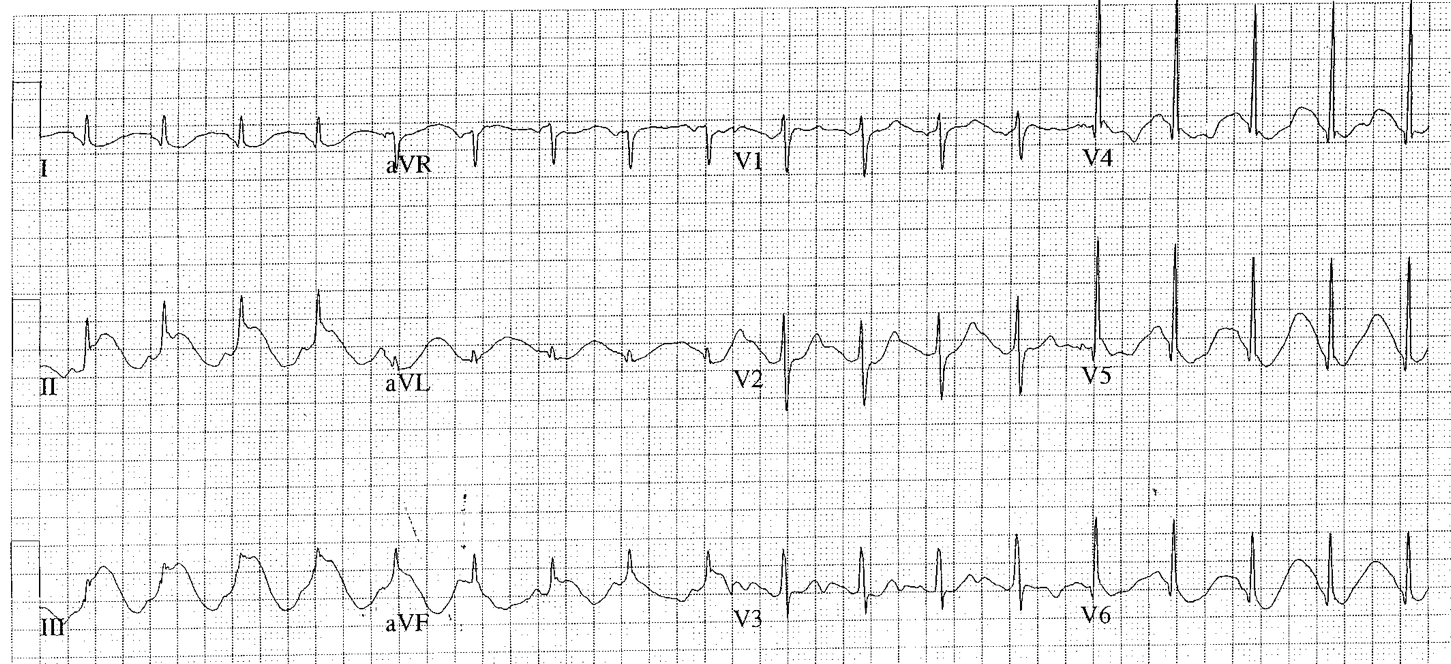
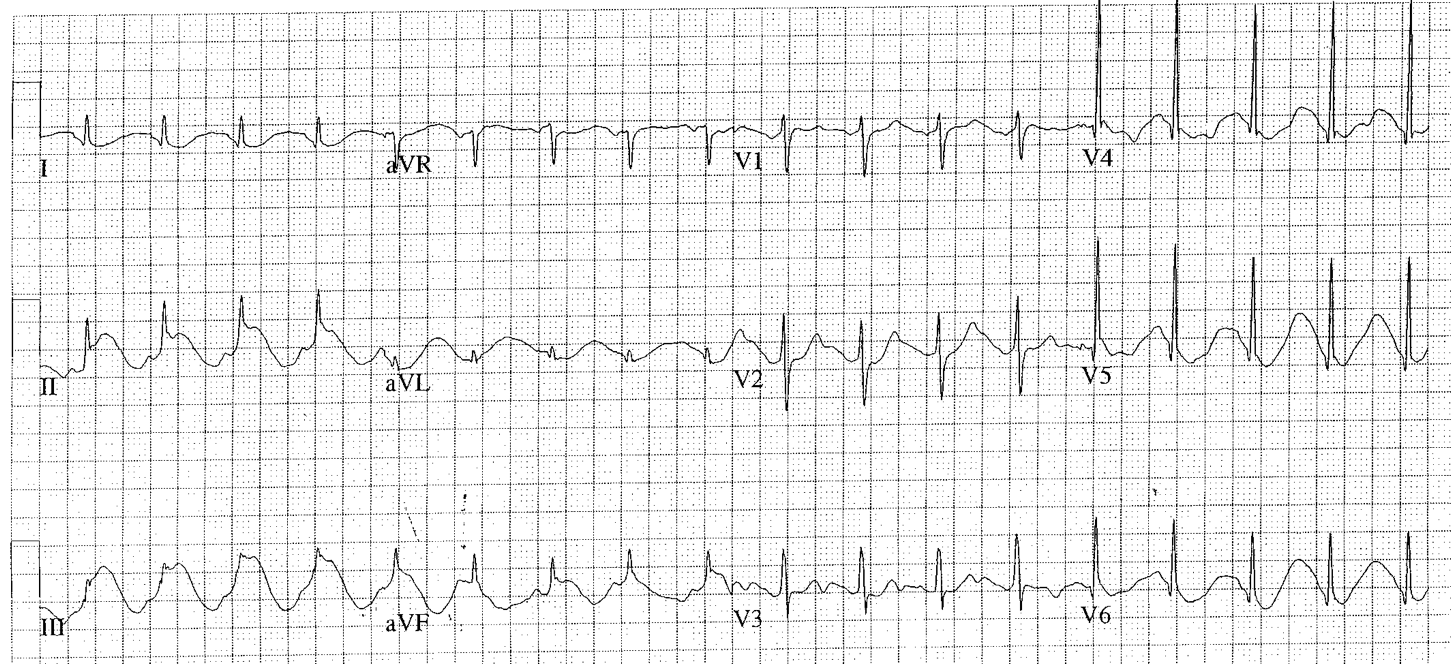
ST Segment Elevation
|
CAUSES OF ST ELEVATION
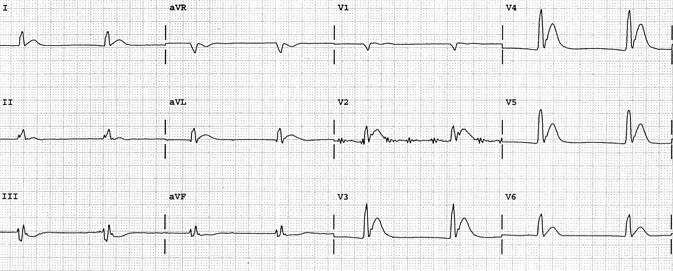
Ischemia, injury, infarction (i - i - i ) Characteristics: chest pain; ST elevation localized to a wall/vascular distribution; Q waves
|
SECONDARY ST ELEVATION
Characteristics: wide QRS complexes or LVH; mirror image of ST depression
Characteristics: wide QRS complexes or LVH; mirror image of ST depression
- LBBB: coved, elevated ST-Ts in leads with downgoing QRS complexes
- WPW: as above
- Paced rhythm: as above
- LVH: upward concave ST elevation and upright Ts in V1-V2 (mirror image strain)
TERMINAL NOTCHING OF THE QRS COMPLEX FOLLOWED BY HAMMOCK-SHAPED ST ELEVATION
- Heart rate fast - pericarditis: diffuse ST elevation; depressed PR segments (esp. in II)
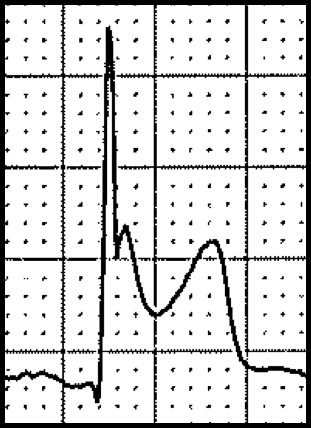
- HR normal - early repolarization: triphasic QRS with terminal notch; upright Ts; normal QT
- HR slow - hypothermia: Osborn wave; prolonged QT; shivering artifact
- Early repolarization variant: early repolarization-type ST elevation followed by inverted Ts – usually seen in AA males with LVH, and with acute or chronic cocaine use
ELECTROLYTE ABNORMALITIES/DRUG EFFECTS
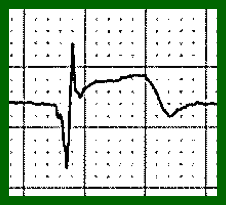
- Hypercalcemia: coved ST elevation and absence of Ts in anteroseptal leads (STs are probably Ts)
- Digitalis: scooped ST elevation in anteroseptal leads; mirror image of scooped ST in lateral leads
- Hyperkalemia: ST elevation in anteroseptal leads; narrow-based peaked Ts; “Brugada pattern”
- Na-channel blocker toxicity: (including TCA, cocaine): “Brugada pattern”
MISCELLANEOUS
- Acute CNS disorder: (SAH, ICH, trauma): QT frequently prolonged
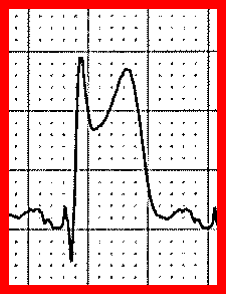
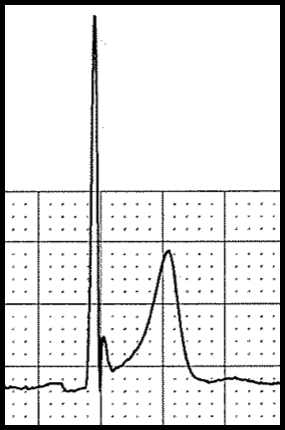
- Brugada syndrome: V1-2: rSR’, coved ST elevation, T (high take-off ST elevation followed by T downgoing)
PSEUDO-ST ELEVATION
- Atrial flutter: regular SVT at ~150/min; flutter waves may mimic ST elevation
- Artifact: ST changes from cycle to cycle (ST elevation does not respect the cardiac cycle)
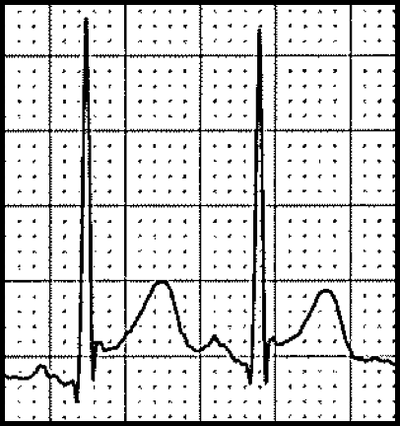
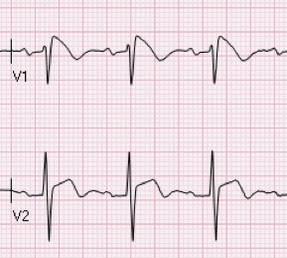
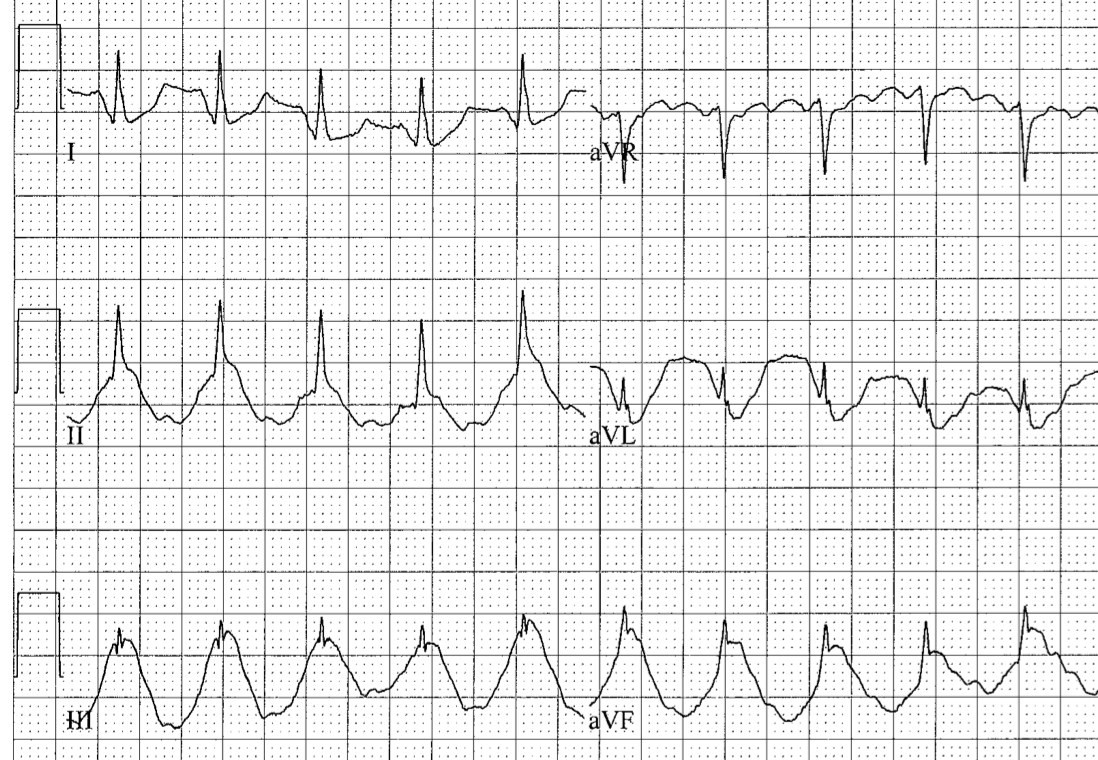
SPIKED HELMET SIGN
- Does respect the cardiac cycle: most likely physiologic signal (repetitive epidermal stretch from increased intracavitary pressure)
- Suggests acute intrathoracic or intraabdominal event
- High risk condition, high hospital mortality
- Recognition of the spiked helmet sign should lead you to search for acute pathology
- If present in the inferior leads, consider acute abdominal event
- If present in the chest leads, consider acute thoracic event
- Prompt recognition may help find and treat the acute non-cardiac condition