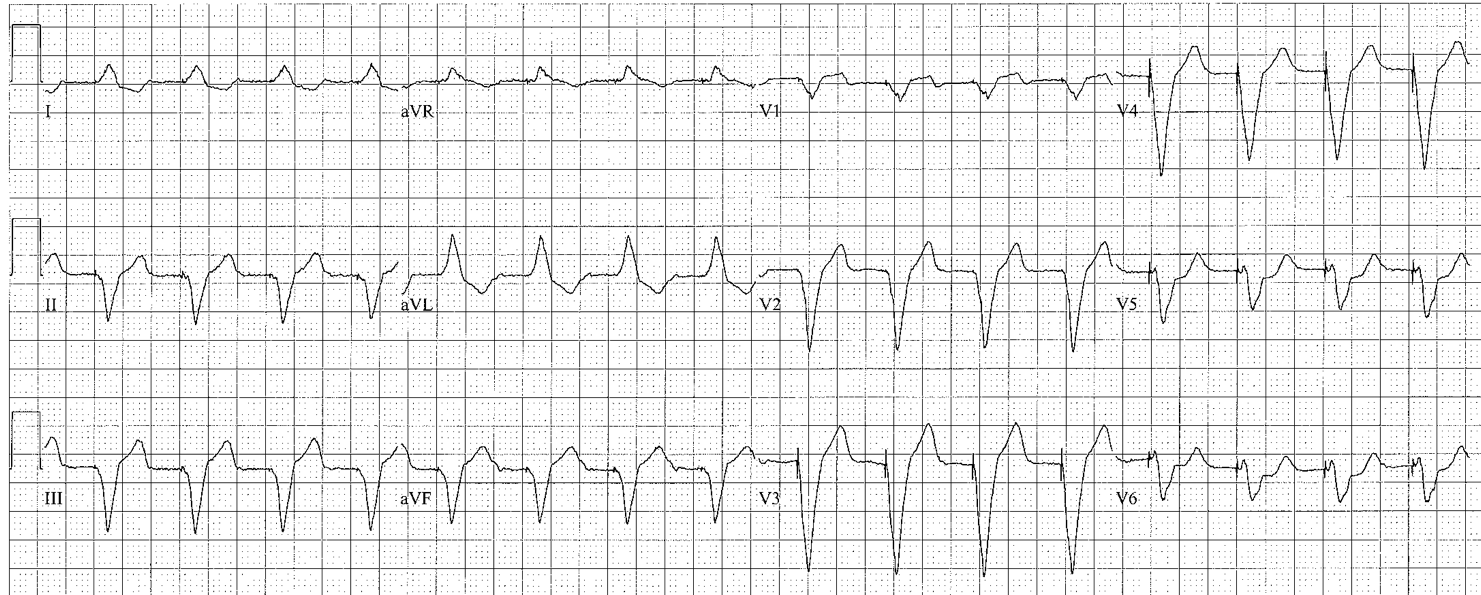
WIDE QRS
No P Waves Present
Ventricular Rhythm
no P waves before QRS complexes
- Regular wide complex tachycardia: 90% ventricular tachycardia
- Dissociated P waves: 100% ventricular tachycardia
- QRS morphology that does not fit a BBB pattern: almost certainly ventricular tachycardia
- If rate is ~70, consider pacemaker rhythm: search for pacer spikes
- < 60/min: ventricular escape (usually 35-40/min) – why? Sinus arrest or AV block
- 60-120/min: accelerated idioventricular rhythm (reperfusion arrhythmia; cocaine; lytes; ICU)
- ≥ 125/min: Ventricular tachycardia
- With ventricular rhythms, the QRS morphology and ST-Ts should not be further analyzed
P waves Present
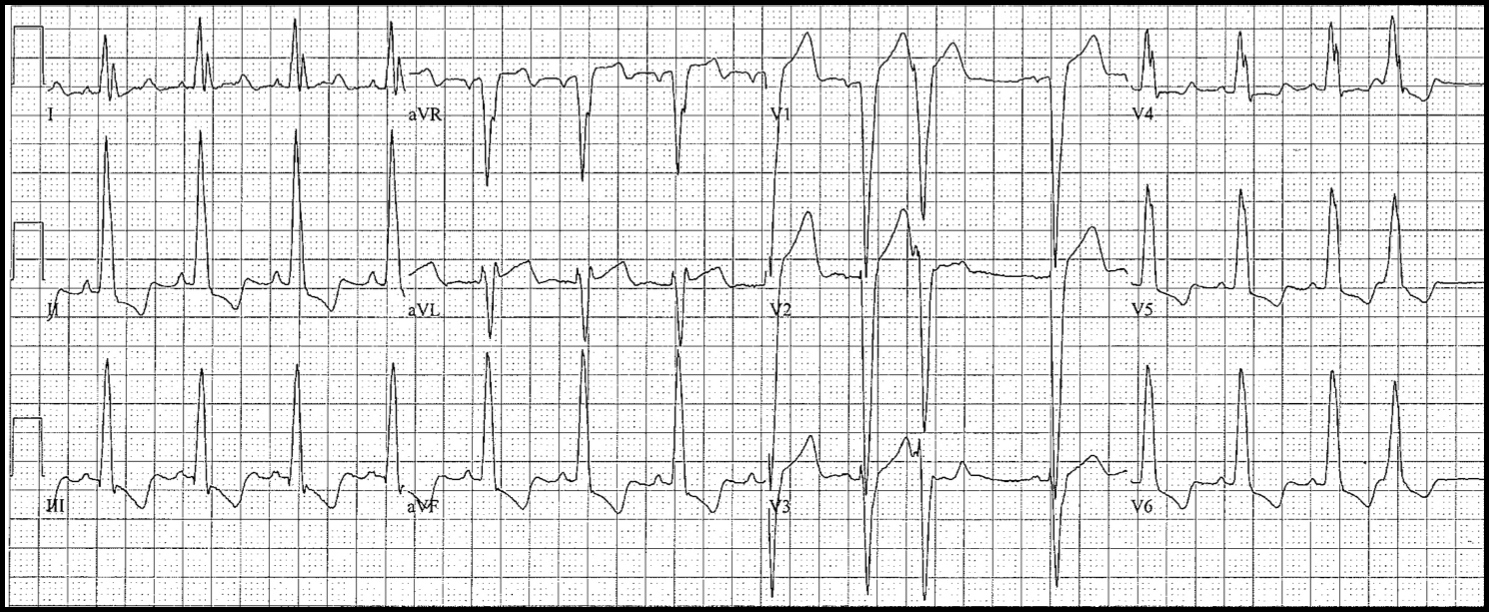
Right Bundle Branch (RBBB)
Diagnostic Criteria
- QRS ≥ 0.12 s
- R is upgoing in V1: triphasic QRS complexes
–typically rSR’
–could be M-shaped
–second upgoing component must be taller and wider than the first - Left leads (I, aVL, V6): deep S waves
- Bifascicular block = RBBB + left anterior or posterior fascicular block
- RBBB does not affect the initial QRS forces: search for pathologic Q waves
- RBBB does not affect the ST segments in the lateral leads:
- You still need to search for possible ischemia
- Expected (secondary) repolarization pattern: ST-T usually down in V1; often down in V2, V3 as well
CLINICAL SIGNIFICANCE
- Isolated chronic RBBB has questionable clinical significance
- no work-up is indicated for chronic RBBB
- New incomplete or complete RBBB
- chest pain, SOB: consider PE
- syncope: consider PE
- STEMI and new RBBB: high-risk condition
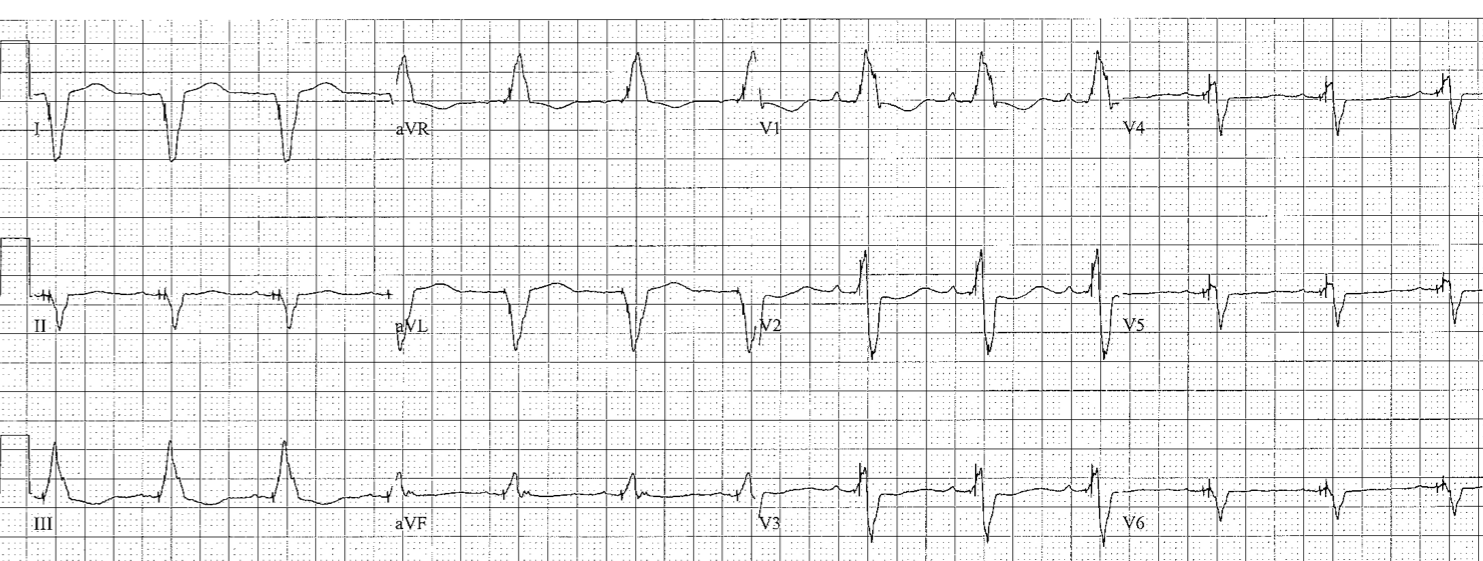
Left Bundle Branch
Diagnostic Criteria
- Left lead (I, aVL and V5 or V6) QRS is predominantly upgoing, slow upslope, absence of q waves
- Right lead (V1 – V3) QRS is predominantly downgoing, trivial or no R waves
- Pathologic Q waves in the inferior leads may signify remote inferior MI
- Pathologic Q waves in several lateral leads may signify remote anterior MI
- ST segment elevation concordant with the QRS complex may signify acute STEMI
- T-wave inversion concordant with QRS complex (Ts ↓ in V1-V3) may signify ischemia
- Expected (secondary) repolarization pattern: ST-T axis opposite to QRS axis
CLINICAL SIGNIFICANCE
- LBBB is frequently associated with structural heart disease
- Left axis deviation: left-sided disease
- Right axis deviation: possibly severe pulmonary hypertension
- Causes left ventricular dyssynchrony
- Poor prognostic indicator in CHF
- Patient may benefit from CRT (BiV pacer)
Wolff-Parkinson-White Pattern
- short P-R intervals (< 0.11s)
- delta waves
- usually does not fit either bundle branch block pattern
- V1 may be either upgoing or downgoing (upgoing in ~60%)
Rv Paced
- I, aVL looks like LBBB
- all chest leads (including V5 and V6) are downgoing
- II, III, aVF are downgoing
Biventricular Paced (BiV-paced)
- QRS in lead I starts down; QRS in V1 usually upgoing
- search for pacer spikes and clinical correlation (does the patient have a pacemaker?)
Nonspecific intraventricular conduction delay
Does not fit any of the above
- frequently coexists with LAE, 1st degree AV block, atrial fibrillation
- several causes: review the company it keeps
- LVH with QRS widening: when LVH criteria are present
- Periinfarction block: when pathologic Q waves are present
- Hyperkalemia: when narrow-based peaked T waves are present
- Hypothermia: when Osborne waves, bradycardia, ST-T abnormalities, long QT are present
- Drug toxicities: when QT prolongation is present (TCA: deep S in I; tall R’ in aVR)
- Infiltrative heart disease and connective tissue disease (e.g., amyloidosis, PSS)