ST-t Patterns
T-QT Pattern (not an established name)
- Large, sometimes global T wave inversion
- T waves may be giant negative; occasionally giant positive
- Prolonged QT
- A stereotypical response to a variety of noxious stimuli
- Usually evolves ~24 hrs after the insult
- Causes:
- Acute CNS disorders (SAH, CVA, thalamic stroke, brain tumor, status epilepticus)
- Catecholamine effect (-adrenergic agonist inotropes, inhalers, cocaine, pheochromocytoma)
- Emotional stress (Tako-Tsubo cardiomyopathy)
- Pulmonary edema
- Massive PE
Clinical Significance
- Most likely common cause: acute adrenergic insult
- ECG evolution: typically evolves “next day”; gradual slow resolution in days or weeks
- Female > male
- Troponin elevation, LV dysfunction common
- Prognosis is benign
- Treatment: underlying condition; b-blocker (except for the asthmatic)
|
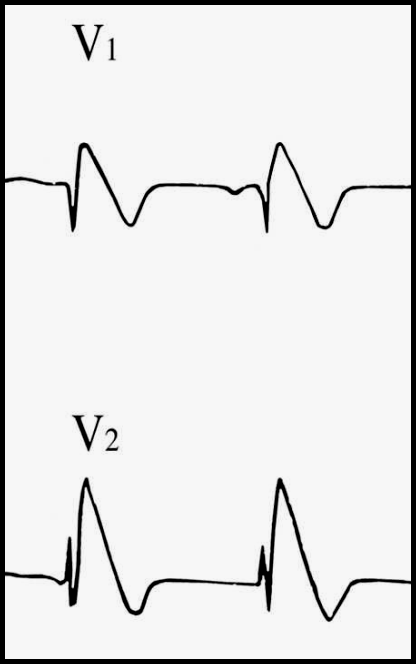
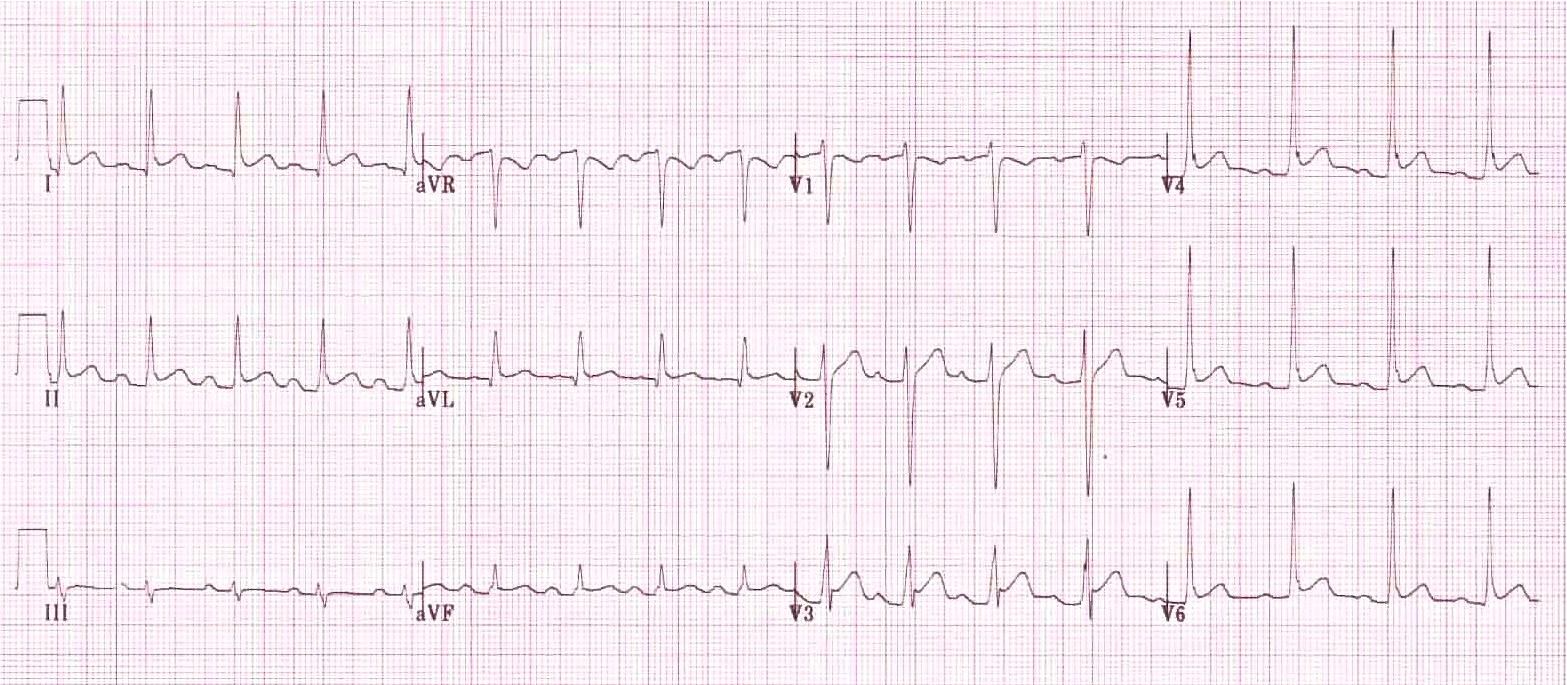
Brugada Pattern
|
Clinical Significance
- The only treatment that can prevent SCD is implantation of an ICD
- The majority of patients with the Brugada ECG are not at a high risk for sudden cardiac death
- In critically ill ICU patient: consider hyperkalemia
- If patient was “found down”: consider sodium channel blocker toxicity
- Risk stratification is crucial
- Resuscitated sudden death (high risk)
- Documented VT
- Personal h/o unexplained syncope
- Family h/o unexplained sudden death at a young age
- Southeast Asian ethnicity
- Asymptomatic (low risk)
Terminal positivity of QRS (terminal notch and hammock-shaped ST elevation)
- “Early repolarization” (normal variant)
- Best seen in V4
- QRS triphasic (up, down, up again)
- Upward concave ST elevation starts from the upsloping QRS (this may cause a notch)
- Normal, upright T waves
- QT is normal
- Hypothermia
- Terminal QRS notch more prominent (Osborn wave or J wave)
- Frequently associated with sinus bradycardia or slow atrial fibrillation
- Marked ST-T abnormalities may be present (both ST and ST)
- Prolonged QT
- When rewarming: shivering artifact
- Pericarditis
- Diffuse ST elevation; ST elevation usually spares aVR and V1
- Usually associated with sinus tachycardia
- P-R segments may be depressed (especially in II) or elevated in aVR